OPS & TRAINING
A MATTER OF MINUTES
04 Jun 2012

When it comes to an emergency, speed and precision are of the essence. If a soldier requires emergency medical attention, the Singapore Armed Forces Medical Corps' (SAFMC's) Emergency Medical Support System (EMSS) kicks in to provide quick and effective aid.
It is perhaps only in an emergency medical situation that the value of a minute is truly appreciated. According to emergency medicine doctors, with every minute that passes without any aid rendered to a person who has just experienced a cardiac arrest, the likelihood of survival decreases seven to 10 percent.
But if the EMSS - based on the international resuscitation protocol Chain of Survival developed by the American Heart Association - is activated, the odds of survival and recovery for victims of heart attack, heat-related injuries and other medical emergencies improve.
The five components in EMSS are: Early Access (to medical attention), Bystander (Buddy) Aid, which includes Cardiopulmonary Resuscitation (CPR), Basic Life Support and Early Defibrillation, Advanced Resuscitation, and Evacuation for Continuing Care.
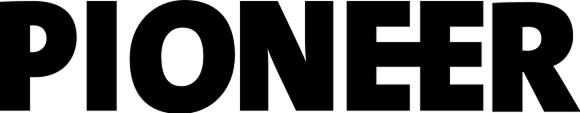
Recruits from Hawk Company learning the steps to CPR during Buddy Aid training at BMTC.
Providing early care
Thousands of recruits pass through the doors of the Basic Military Training Centre (BMTC) each year.
As part of their training, recruits are taught to recognise and provide first aid for heat injuries, burns and fractures during Buddy Aid, a basic soldiering skill module. They also learn to recognise signs of choking and perform the Heimlich Manoeuvre among other basic first aid skills.
Training in CPR and Automated External Defibrillator (AED) was added to the Buddy Aid syllabus in August 2010. This means that recruits are now equipped with the know-how to administer chest compressions to fellow soldiers in an emergency.
"Learning to perform CPR and the use of AED are important life skills where ordinary people can make a difference in medical emergencies," said Lieutenant Colonel (Dr) Gan Wee Hoe, Head of General Staff at SAFMC. He coordinates medical support operations in the SAF and oversees the operational readiness of the SAF's medical forces.
"Training all recruits in these skills enhances the first responder network within the SAF. What it means is that the majority of SAF personnel are now able to administer critical first aid anytime, anywhere."
After going through the training, recruits receive a certificate that states that they are CPR and AED-trained. Valid for two years, the certificate means that recruits are ready to administer early care for the entire duration of their full-time National Service term.
For Specialist Cadet Trainee Joshua Lui, who graduated from BMT in October last year, CPR is an invaluable skill.
The 22-year-old said of his learning experience: "It was rather simple (to learn). The instructors broke it down and we had a lot of hands-on practice. CPR can make a difference between life and death, and being trained in CPR has given me the assurance that I can be of help when the need arises."
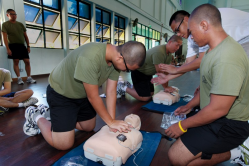
Medics performing basic life support procedures on a patient-simulator mannequin in this simulated emergency scenario.
Basic life support
The next step in EMSS is providing basic life support - a set of procedures performed to sustain life in the event of sudden collapse. Administered by the medics when they reach the casualty, these procedures include rapid defibrillation and introducing air into the casualty's lungs through CPR and an oxygen resuscitator.
To enable medics to better respond to medical emergencies, the SAF has been partnering the Justice Institute of British Columbia (JIBC) since 1996 to run the three-month Basic Combat Medic course.
The curriculum, which entails training medics in first aid and basic life-saving skills, was enhanced in September 2009 and renamed the Emergency Medical Technician (EMT) course. JIBC is one of the world's leading educators for training pre-hospital care paramedics.
Apart from strengthening their basic medical knowledge, the course trains medics to diagnose and administer treatments for conditions such as chest pains and life-threatening allergic reactions.
This ensures that frontline health-care workers in the SAF are equipped with essential medical knowledge and clinical skills which are up to date, relevant and effective in treating the range of medical emergencies that they are likely to encounter in the SAF, said LTC (Dr) Gan.
The SAF's ambulances were upgraded in 2010 and boast a larger capacity compared to the older vehicles.
Advanced life support
After basic life support treatment is administered on site, the casualty is quickly transported to the nearest emergency medical facility.
"In medical emergencies, the fastest access to an emergency resuscitation facility is critical. This can be either the nearest resuscitation facility in the hospital's emergency department, or the Emergency Resuscitation Facility (ERF) of the SAF medical centre. When the situation dictates, we will utilise the fastest means to bring the injured soldier to the nearest hospital by land or air," explained LTC (Dr) Gan.
To ensure that casualties receive advanced resuscitative treatment without delay, all SAF medical centres have an ERF.
With its advanced resuscitation equipment and medications, the ERF is where the Medical Officer (MO) performs critical procedures on the casualty to maintain an open airway, support his breathing, administer fluid resuscitation and ensure that oxygen is circulated to the rest of his body.
Evacuation for continuing care
The EMSS is supported by the SAF's own ambulance fleet with accompanying medical personnel. Advanced and modern resuscitation and monitoring equipment on board the SAF ambulances allows medical personnel to continue treatment and monitor the casualty's vital signs on the way to the hospital.
But what if the casualty is located at an offshore location like Pulau Tekong? For these contingencies, personnel from the Republic of Singapore Air Force's 125 Squadron (SQN), 126 SQN, 127 SQN and 1 Medical SQN (1MS) stand ready round-the-clock to perform medical evacuations by helicopter, also known as heli-medevac.
EMSS Chain of Survival
"Scramble" is an aviation term used to describe real-time activation for contingency operations. When the crew from 125 SQN hear the scramble call, two pilots and two aircrew specialists rush to start up the Super Puma helicopter on standby for heli-medevac.
Flying to the rescue
One Super Puma helicopter pilot who understands the intensity of a heli-medevac first-hand is Captain (CPT) Peck Beng Hwee, who has been a Search and Rescue (SAR) pilot with 125 SQN since May 2009.
The 33-year-old remembers his first local scramble experience, which took place during a 24-hour shift at Sembawang Air Base in February 2010, in vivid detail.
"When we heard the alarm ring, I felt an adrenaline rush and all the training we had undergone sort of took over. We took our equipment and rushed to the aircraft. A life was at stake and the casualty was waiting for us," he recounted.
Two pilots and two aircrew specialists are involved in each heli-medevac operation; the latter are also known as the winchman and the winch operator.
When the scramble alarm is sounded, they rush to start up the Super Puma helicopter that is on standby for SAR operations, aided by three ground crew members. Once the MO and medic arrive, the helicopter lifts off, all in a matter of 15 minutes.
"Fifteen minutes is just a guide. As fast as the aircrew, MO and medic can make it, we want to move off to reach whoever's in need as soon as possible, because every second, every minute is time wasted in a life-threatening scenario," said CPT Peck, who added that for the last few scrambles, the crew took off within 10 minutes of the alarm.
Working together
In situations where there is no suitable landing area, such as over open seas or in the forests, the winchman and winch operator step in to lift the casualty safely onto the aircraft.
Connected to the starboard (right) side of the aircraft, the winch is a retractable steel cable hoist with a 600-pound (270kg) lift. The winchman is first lowered to the casualty, followed by the MO, who provides an initial medical assessment. Thereafter, the casualty is hoisted onto the aircraft together with the winchman, before the MO is lifted.
The other aircrew specialist - the winch operator - guides the winch and provides inputs to the pilots if they are off position. The latter are not able to see what goes on below, and manoeuvre the helicopter to hover at a specific spot, using reference points and instructions from the winch operator.
Care in the air
Working closely with the pilots and aircrew specialists for each heli-medevac are the MOs and medics from 1MS.
Medical equipment on board the Super Puma helicopter includes a stretcher, oxygen tanks, a defibrillator and a monitoring unit to check vital signs.
Armed with the equipment in the MO's and medic's bags, which includes resuscitation medications and tools like the endotracheal tube which helps keep a casualty's airway open, the MO and medic work hand-in-hand to ensure that the casualty's condition does not worsen.
Said combat medic specialist 3rd Sergeant (3SG) Chew Jing Wei: "We have to work in a confined space, so we have to be very calm, make sure that the casualty and our equipment are well-managed, and be prepared for unforeseen circumstances."
To prepare for SAR operations, medical personnel undergo mock-up drills weekly. "The MOs regularly take the medics for Crash 1 tests, which are mock-ups of the casualty scenario.
We go through the whole simulation, what is going on with the patient and why his condition is deteriorating. By doing this, the MO gets to know the capability of each medic better and how they perform under stress," explained CPT (Dr) Victor Liang, who has been on two scrambles since joining 1MS in August last year.
He may be operating from within the confines of a helicopter, but the equipment the SAR MO carries in his bag, like the endotracheal tube and Laryngeal Mask Airway, enables him to support the casualty's breathing en route to the hospital.
Ensuring standards
The SAF's EMSS was endorsed by the SAF Emergency Medicine Specialist Advisory Board (EM SAB) in its latest review which took place in October last year.
The board, which comprises senior, authoritative emergency medicine and trauma surgery specialists from the public health-care sector, is chaired by Associate Professor Eillyne Seow, who is Divisional Chairperson of Ambulatory & Diagnostic Medicine at Tan Tock Seng Hospital, and a Senior Consultant in Emergency Medicine.
The role of the board is to review the SAF's emergency medical response policies and strategies regularly. This ensures that its practices are modern, up to date and benchmarked against international best practices.
At the same time, the board also reviewed and endorsed the mobile medical evaluation team or MobileMET, an initiative by SAFMC to improve the evaluation of frontline health-care personnel.
Comprising assessors from the Military Medicine Institute, the MobileMET tests individual and collective emergency medical response in the field and the ERFs at the medical centres.
Emphasising that the inter-component linkages in EMSS are important, LTC (Dr) Gan said MobileMET helped to test the transition of care between the different components of the EMSS chain of survival.
All of the SAF's medical centres passed the inaugural MobileMET audit, which took place from last October to March this year. An emergency response medical team from each medical centre was evaluated on a checklist of emergency care steps in areas such as evacuation procedures, resuscitation skills and drug administration.
Dr Seow found this initiative admirable. "MobileMET makes sure those EMSS links are practised," she said.
The evaluation process is recorded and lessons learnt are shared with the rest of the medical centres. Trainers like Military Expert 3 Lim Hock Cheong are also invited to observe the assessment, which helps them to better understand how the knowledge taught at the SAF Medical Training Institute is applied in reality.
The 51-year-old, who has had 20 years of experience training combat medics, said: "MobileMET allows me to see how our men perform in an emergency case, to know what their strong and weak points are and to do corrections on the spot to deal with the situation. It's a very good training platform for me and for the trainees."
Dr Seow agrees: "The feedback loop is very good. If you can gather all the lessons you learn in all SAF medical centres, and share and validate these lessons, the whole organisation goes up a notch."
Emphasising that the SAF is committed to providing a high standard of medical care for soldiers during training and operations, LTC (Dr) Gan concluded: "We have been, and will continue to work with external subject matter experts and hospital specialists to review and enhance our EMSS.
"The outcome of this systematic review is to continually strengthen our system's capabilities and enhance the professional training and competency of our people."
SAF Emergency Medicine Specialist Advisory Board
The board is chaired by Associate Professor Eillyne Seow, Divisional Chairperson of Ambulatory & Diagnostic Medicine at Tan Tock Seng Hospital.
Other members include:
- Assoc Prof Lim Swee Han, Senior Consultant, Department of Emergency Medicine, Singapore General Hospital (SGH)
- Assoc Prof Kenneth Mak, Chairman of the Medical Board at Khoo Teck Puat Hospital (KTPH), and Director of Jurong Medical Centre
- Assoc Prof Mark Leong, Head of the Department of Emergency Medicine, SGH
- Dr Francis Lee, Head of the Department of Acute and Emergency Care, KTPH
ALSO READ IN OPS & TRAINING

Exercise Wallaby 2025: To see better, shoot faster
31 Oct 2025
The SAF focuses on complex strike missions and multi-domain integration in Exercise Wallaby 2025, the 35th edition of its largest unilateral overseas exercise.

Ex Wallaby 25 – Greater Integration and Complexity
25 Oct 2025
The 35th edition of the SAF’s largest unilateral overseas exercise is an opportunity for expanded scale and deeper integration towards an effective, networked fighting force.

Ex Forging Sabre ramps up use of unmanned assets in integrated strike operations
12 Sep 2025
In this 10th edition of Exercise Forging Sabre, the SAF sharpened its cutting edge for the dynamic modern battlefield, with expanded integration between manned and unmanned platforms.